Death By Dehydration In ICU
COVID-19 ICU patients get higher dosages; ICU consultant ignores VITT
Disclaimer: This does not constitute medical advice, speak with a medical professional.
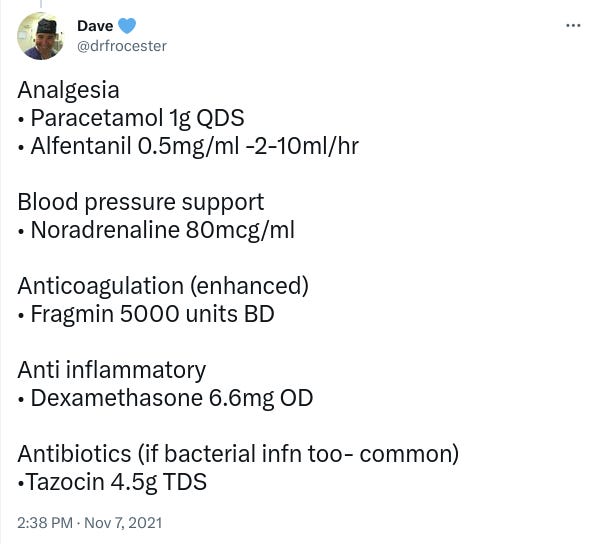
On November 5th 2021, one ICU consultant posted a photograph of drugs supposedly given to COVID-19 patients in critical care (read: Intensive Care Unit; ICU; also known as ITU or ‘critical care’), in one day, whilst also trying to promote vaccines:
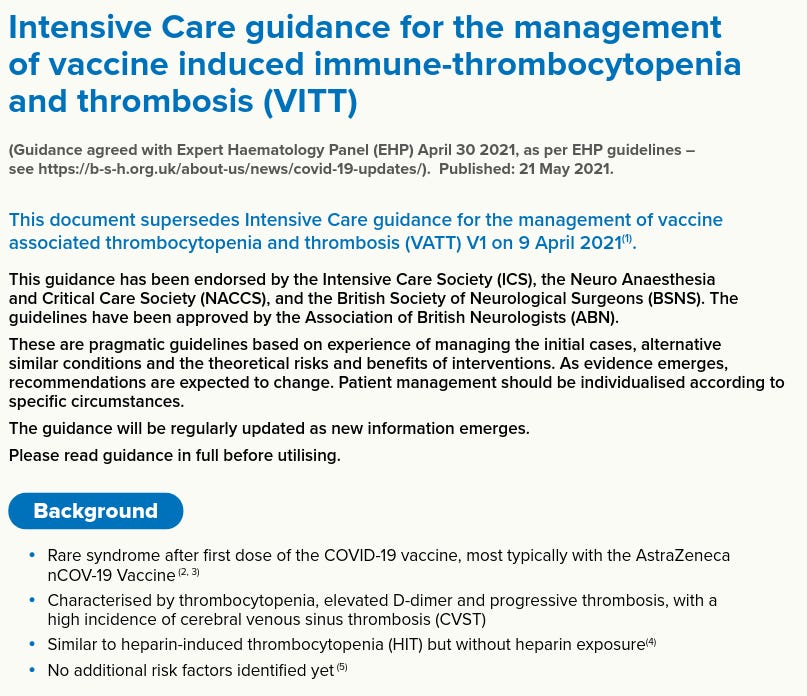
In their constant beratement of the unvaccinated, perhaps they forgot the notice posted by the Intensive Care Society (ICS) — advisers of ICU in the NHS — back in April 2021. It shows a 25-30% mortality rate for vaccine-associated thrombocytopenia and thrombosis (VATT, AKA VITT) in UK cases admitted to ICU:
The ICS would publish again similarly, in May 2021:
The documentation recommends the total avoidance of heparin class anti-coagulants in treating VATT/VITT:
Guidance from December 2020 — before the vaccine rollout — still recommended heparin class anti-coagulant for use in ICU. It does not appear to be updated:
The Pfizer Fragmin (dalteparin sodium), listed by the ICU consultant, is a heparin class anti-coagulant:
Receipt of Fragmin thus might be a problem if you’re vaccinated, at risk from VATT/VITT and have COVID-19 in ICU.
For those who don’t speak medical acronym, per British National Formulary:
OD: “Omne die” - once a day
BD: “Bis die” - twice a day
TDS: “Ter die sumendum” - to be taken three times daily
QDS: “Quater die sumendum” - to be taken four times daily
Perhaps they meant TID (“ter in die”; three a day) rather than TDS? Not clear how an unconscious patient can ‘take’ something. Note all drugs shown in original image are injectable form.
Higher Dosages For COVID-19 Patients
Dr. Pezhman Mehrabian, an ‘interventional chronic pain physician’, asked the ICU consultant why there is so much Alfentanil (opioid), if there’s Propofol (general anaesthetic) and Midazolam (sedative).
‘Dave’ argued COVID-19 patients require “huge amounts of sedation c.f. to a ‘usual’ ICU patient” [c.f. is short for ‘conferatur’, Latin for ‘compare’; compared]. He doesn’t explain why.
ICS guidance repeats the claim similarly, but does not evidence it:
The dosages he specifies in the Tweet above, are found in ICS guidance itself.
German Journalist Tibor Martini, complete with government backed Ukrainian flag, also seemed surprised at the high amount of drugs imaged:
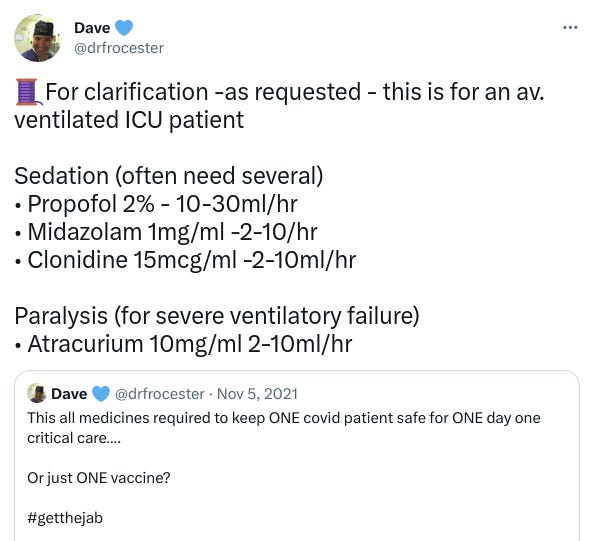
The ICU consultant confirmed this is what they give an “average covid patient”, also compiled with the “senior sister”, specifying the NHS Trust region, Gloucestershire.
Not Solo
In FOIA, Gloucestershire Hospitals NHS Foundation Trust confirmed that they used Intensive Care Society (ICS) guidance as the basis for ICU:
This means ICUs across the UK give higher dosages of drugs to COVID-19 patients.
Alarming, given evidence of PCR fraud regarding SARS-CoV-2 detection. Where are the numbers Substack by Professors Martin Neil and Norman Fenton expand upon the issues with PCR tests raised by The Daily Beagle.
The ICU consultant admits a year later, in June 29th 2022, maybe it’s “with covid” rather than ‘of COVID’ (although this feels like cope for his vaccinated friends ending up in ICU):
If COVID-19 isn’t the main illness, or worse, positive results are fraud, should patients really be receiving ‘higher dosages’ of drugs at all? The Daily Beagle could not find justification or evidence for requirements of higher dosages for COVID-19 patients; perhaps medical experts could show us?
Image Analysed
The Daily Beagle painstakingly isolated and identified every drug and product shown in the image, including dosage amounts. The full list of analysed images has been compiled into a downloadable PDF.
For brevity, most won’t be covered in this article, although we do encourage medical professionals to review our findings and leave feedback in the comments.
Some dosages were inferred based on external resources.
For example, UK’s electronic medicines compendium only mentions 2.5ml, 5ml and 25ml sizes for Atracurium Besilate, which in image is similarly sized to Norepinephrine marked 4ml, meaning Atracurium Besilate ampoules must be between 2.5ml to 5ml. We chose the lower dose of 2.5ml for benefit of the doubt.
Red lines indicate source of information in image (if applicable). Blacked out areas in images are portions not relevant to analysis, and are obscured to avoid confusion.
Tocilizumab isn’t shown in the image, despite being listed in “COVID-19 rapid guideline: Managing COVID-19”.
In a reply to a deleted tweet, the ICU consultant remarks “All the patients received all available treatments prior to ICU - dexamethasone, tocilizimab, oxygen, cpap etc”.
Seems like a contradiction to REMAP-CAP findings on timings, which advises within 24 hours of entering intensive care, not before:
Results from the government-funded REMAP-CAP clinical trial published today showed tocilizumab and sarilumab reduced the relative risk of death by 24%, when administered to patients within 24 hours of entering intensive care.
Although dual antibiotic Piperacillin/Tazobactam is used; Piperacillin is a bactericidal that interferes with bacterial cell wall synthesis, and Tazobactam is a type of sodium that kills β-lactamases bacteria, it is not a IL-6 inhibitor like tocilizumab or sarilumab, and it is odd neither IL-6 inhibitor is included in ICU treatment.
Midazolam Listed
The usage of Midazolam (a benzodiazepine) here is a double-edged sword. It has been argued that in theory it is used for sedation prior to ventilation, but ICS documentation for COVID-19 does not mention this, nor has The Daily Beagle seen evidence of this indication.
That said, the ICU consultant claims Midazolam is used for ventilated ICU patients:
In ICS guidance “COVID-19 rapid guideline: Managing COVID-19”, it mentions many of the same drugs we saw in the Midazolam murders, including lorazepam, haloperidol, and of course, midazolam itself. The claimed treatment target is ‘anxiety, delirium and agitation’, not ‘intubation’ (an encompassing word that also covers ventilation).
At the bottom it mentions doses are based on ‘palliative’ (end-of-life) and talks about higher dosages. Note this is for those 18 years and over (not just the elderly).
Midazolam and Morphine are also mentioned but for ‘breathlessness’. Again, no mention of ‘intubation’:
At the bottom, it repeats the unevidenced mantra that “higher doses may be needed […] in people with COVID-19”.
According to NICE (National Institute for Health and Care Excellence), breathlessness has many and varied causes (heart issues, lung problems, iron nutrition, etc), but they stress the subjective nature of it:
NICE are the same organisation who published the dubious and now withdrawn NG163 guidance mentioned in the Midazolam murders where it told medical professionals to ignore fears of causing respiratory depression with Midazolam.
The Daily Beagle found another issue with the imaged products as well.
Salt Levels Are Too High
Salt, also known as ‘sodium chloride’; or ‘natrium’ in Latin. 90% of sodium consumed (from all sources) is excreted in urine. Most of the rest is by sweat.
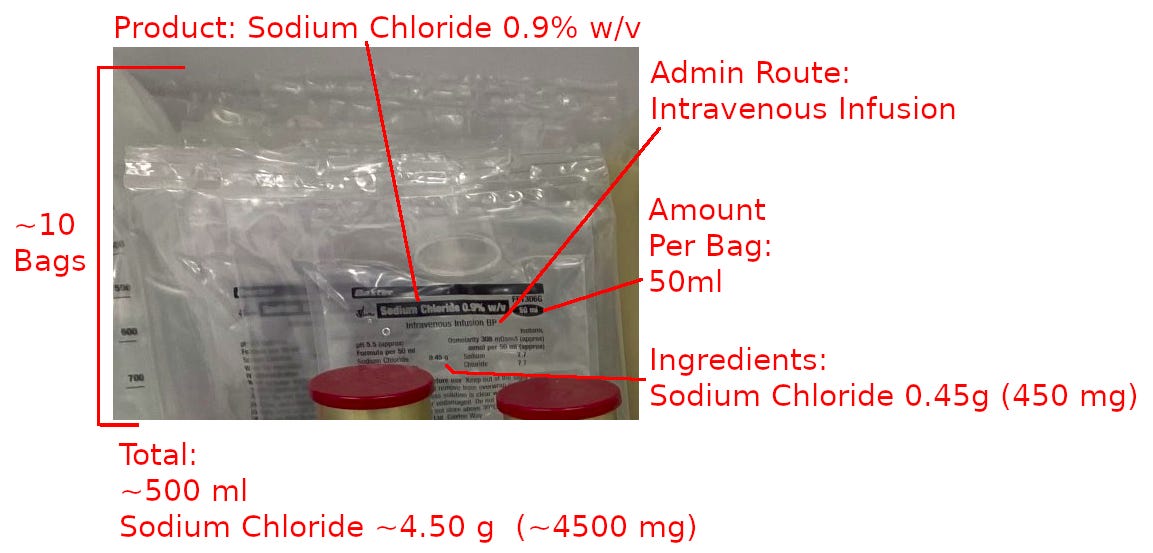
Two sources of salt are shown in-image: saline (lit. salt water) bags and electrolyte bags (PlasmaLyte).
By our calculations a patient is receiving a whopping 15.02g of salt a day. According to the NHS itself, adults should eat no more than 6g of salt a day:
It’s not clear how much salt is safe to give via intravenous feed but this seems like a lot. Why so many saline bags? They’re typically used to dilute the drugs. This piggybacks COVID-19 patients being given more drugs: more drugs, more saline.
Pipercillin dilution calls for a 50mL bag of 0.9% saline. It’s worth bearing in mind Tazobactam is also sodium, and thus Piperacillin also contains sodium (see below image).
Another term for too much salt is hypernatraemia (hyper - over, above; natr - short for natrium; aemia - in blood; lit. too much salt in blood).
Nuturing Hypernatraemia
There are three main causes for it:
Hypernatraemia represents a deficit of water relative to sodium and can result from a number of causes, including free water losses, inadequate free water intake, and, more rarely, sodium overload.
Not drinking enough water, losing too much water, or given too much salt.
Another study details more directly:
[…] hypernatremia usually develops only when there is no access to free water, when the person has a disturbed sensation of thirst or when he or she is unconscious.
Read: patient denied access or unable to get water; patient unable to sense thirst (E.G. due to illness or drugs), or patient is too unconscious to drink (read: sedated).
Curious parallels to Midazolam murders. Midazolam is a sedative: sedated patient can’t drink of their own free accord. Care homes have a history of elderly patients dying of dehydration. Lets not forget the drugs that dry them out too.
How Do Patients Dehydrate In ICU?
Medical professionals might be confused. Surely with 0.9% saline bags, patients are getting all the normal fluids they need? 0.9% is supposed to be the right balance, right?
For the layperson, >145 mmol/L of sodium in the blood is classified as hypernatraemia. So anything above 145 mmol/L is too much.
For medical professionals: 0.9% saline bags — standard issue in most hospitals — clock in at 154 mmol/L. 9 mmol/L above the 145 mark for blood. So small almost no-one would notice.
Ironically called ‘isotonic’ saline. Isotonic is supposed to mean something that won’t cause a net flow of water into or out of a cell (via osmosis differences caused by salinity). Salt difference compared to blood make it hypertonic.
Inversely, the other common bags, 0.45% saline — exactly half — used to treat hypernatraemia, are too little (~77 mmol/L), leading to hyponatraemia (hypotonic). To get a more stable 142 mmol/L, it would roughly need to be a 0.82% saline bag.
For the interim, it may be possible to achieve roughly ~134 mmol/L with three 0.9% saline bags mixed with one 0.45% saline bag.
Death By Dehydration
The Daily Beagle found hypernatraemia — implying dehydration — was common in ICU.
One study looking at SARS-CoV-2 patients found those ending up in ICU experienced far more hypernatraemia (>30%) than test-negative patients (remember the PCR fraud):
Hypernatremia was significantly more frequently observed in COVID-19 patients, in 38% (74 of 193), versus only 8% in SARS-CoV-2-negative patients (11 of 138) (p < 0.01) […]
Same study, higher percentage of those that died had experienced dysnatraemia (either too little or too much salt in blood) than those who didn’t die:
[…] 71% (32 of 45) of the deceased COVID-19 patients developed dysnatremia (hyponatremia, hypernatremia or both) versus 57% (84 out of 148) of the surviving COVID-19 patients.
Another study found dehydration made respiratory illness worse:
Dehydration of the upper airways increases risks of respiratory diseases from COVID-19 to asthma and COPD.
Another argued in relation to SARS-CoV-2 there was a 2.4 fold increase risk of death involving hypernatraemia:
Hypernatremia was detected in 83 (76.1%) of the patients who died, with a cumulative reduction in survival (p < 0.01) and an increased risk for death by 2.4 fold (95%CI 1.4–2.9).
Another study, titled “COVID-19 symptoms are reduced by targeted hydration of the nose, larynx and trachea” argues hydration of the respiratory system aids against COVID-19 symptoms, although this is a general context, and not specifically to ICU.
One argument someone could make is, maybe SARS-CoV-2 increases water losses. Is this true (even if we ignore the possibility of PCR fraud)?
Happens Regardless Of Disease
One study from 2016, before the SARS-CoV-2 events occurred, remarked hypernatraemia was rare in non-ICU patients:
[…] hypernatremia is rare in noncritically ill, hospitalized patients with a prevalence of 0·2% […]
Comparing it to ICU, it then finds:
In contrast, hypernatremia is a much more common finding in critically ill patients treated in intensive care units (ICUs).
Detailing (emphasis added):
[…] almost all patients who have ever experienced hypernatremia during their ICU stays developed this electrolyte disturbance during their first week after admission […]
It alarmingly concludes (emphasis):
Hypernatremia is a common and largely preventable complication of intensive care.
Another study from 2011 remarked patients in ICU were at high risk of hypernatremia due to their inability to freely drink water due to sedation and ‘fluid restriction’:
Critically ill patients in ICU are at high risk of hypernatremia because of their inability to control free water intake as a result of sedation, intubation, change in mental status, and fluid restriction for various other reasons.
Another study from 2020 also points the finger at ICU treatment methodologies:
Since the median admission serum sodium levels were well beneath 145 mmol/L [read: they had normal salt levels before entering ICU], we can postulate that overly restrictive ICU fluid intakes may lead to dehydration, which in our study was present in 52% of the patients with ARDS due to SARS-CoV-2.
This isn’t a small potatoes problem either; dehydration leads to much longer stays in ICU…
ICU stay was longer (19 vs 6 days) in patients with compared to those without hypernatremia […]
…longer stays in turn increase the risk of death:
Other factors also associated with death were long length of stay (LOS) (HR:1.54; 95%CI:1.21–1.78), old age (HR:1.63; 95%CI:1.28–1.88), and kidney disease (HR:1.77; 95%CI:1.21–3.30).
As another study notes, as soon as a patient is transferred out of ICU, they started to recover from hypernatraemia:
Following transfer to an in-hospital intermediate care unit or an outside hospital ICU, hypernatremia gradually resolved with improving overall condition.
This isn’t isolated, but frequently occurring, in numerous countries. Increases risk of death 2.4 fold, yet has zero coverage despite peer-review papers, it has not been properly addressed.
Enter Ventilators
Another cause of dehydration (and thus hypernatraemia) are ventilators. The earlier study from 2020 also highlights issues of moisture loss from ventilators:
During mechanical ventilation, the upper airway is bypassed by orotracheal intubation and thus cannot contribute to the natural heat and moisture exchange process of inspired gases […]
The lungs emit approximately 25% of daily total water mass loss in the process of hydrating inhaled air […]
Worsened by ventilators bypassing bodily cycle of heat exchange.
Yes, some ventilators can have heat exchangers and humidifiers installed, but it isn’t always applicable, nor is it always used. In the study, “managing humidity support in intubated ventilated patients with coronavirus disease 2019 (COVID-19)” it notes that:
HME [heat and moisture exchanger] is not recommended for use in patients with copious, thick secretions or low tidal volumes, which have been associated with mechanical ventilation of COVID-19 patients.
Excess mucus can block lungs, cause tubes to get clogged and risk bacterial infection. More water vapour in ventilators means lungs have to work harder to breathe air:
[…] the work of breathing was greater in the HME group, possibly due to increased resistance to gas flow […]
Typically means dry, cold air extracting moisture from warm lungs (hot air can hold more moisture than cold air). There’s one other, less expected culprit to hypernatraemia…
Air Conditioning
In one image the ICU consultant shows an image of a vent in the ceiling above a patient bay in response to an earlier tweet (patient bay indicated by hanging drip feed):
Air conditioners are good for comfort. Except cool air means patient doesn’t sweat as much, if at all. One of the few ways a person can lose salt besides urine. Reduced expenditure of salt in sweat means the patient retains higher salt levels. A subtle cause, but worth noting.
ICU Drugs Induce Delirium And Impede Drinking
A former ICU patient remarked how ICU drugs induced delirium (a sort of hallucinogenic state of mind), where nothing makes sense:
Even if ICU patients are not sedated, they may not have the correct state of mind to comprehend what is and is not drinkable water. Thus causing dehydration.
Hypernatraemia Causes Hyperventilation
And to close the circle, hypernatraemia can cause hyperventilation:
This is of course, one possible type of ‘breathlessness’, which forms yet another death spiral (more applicable in care homes) with Midazolam.
This trend of hypernatraemia (thus, dehydration) was surprisingly difficult to spot, and required extensive research and analysis to uncover, including possible causes and reasons why.
This is why this article took so long to publish (this is the fourth re-write). We did ask a few others to review our findings but they weren’t able to offer any insights. Hopefully members of the medical community can weigh in on our findings.
Subscribe for free to get more content from The Daily Beagle.
Learned something important? Share with others so they can learn too!
And leave a comment below:



























I remember a soldier in the Iraq (?) war that was investigated, charged, found guilty and imprisoned for helping a mortally wounded enemy combatant to “shuffle of this mortal coil” ... he was a professional, should have known better and hadn’t, so far as i know, sworn to not kill anyone.
A remarkable piece of research. Thank you.